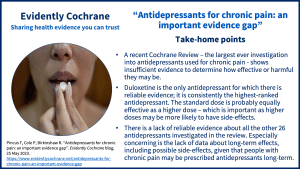
A recent Cochrane ReviewCochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. – the largest ever investigation into antidepressants used for chronicA health condition marked by long duration, by frequent recurrence over a long time, and often by slowly progressing seriousness. For example, rheumatoid arthritis. pain – shows insufficient evidence to determine how effective or harmful they may be. In this blog, principal investigator Professor Tamar Pincus explains the findings, and a clinician (Dr Peter Cole), an anonymous patient, and a researcher (Dr Hollie Birkinshaw) share their reflections.
Take-home points
How our investigation into antidepressants for chronic pain all began…
Some years back I [Tamar] was giving a talk to clinicians in a large pain management department in a hospital. I asked: “How many patients arrive on long-term antidepressants?”
The participants exchanged looks as if I asked a foolish question, and finally one replied: “pretty much all of them”.
“is their pain well-controlled”? I asked.
Vigorous head shakes.
“do they mostly have low mood?”
Unanimous nods.
“Well,” I thought, “I wonder how well these drugs work?”
What we set out to find out
We already knew that there were dozens of trialsClinical trials are research studies involving people who use healthcare services. They often compare a new or different treatment with the best treatment currently available. This is to test whether the new or different treatment is safe, effective and any better than what is currently used. No matter how promising a new treatment may appear during tests in a laboratory, it must go through clinical trials before its benefits and risks can really be known. of antidepressants in specific pain conditions. We wanted to do a review that offers an answer to ALL people living with chronic pain, from any condition, on any antidepressant, of any dose.
We knew we had to include more than just pain intensity as an outcome – patients have told us that reducing pain is incredibly important, but equally important is improving mood, sleep, and physical function. We set out to carry out the largest ever review of antidepressants in chronic pain, and to do it meticulously. Throughout the review, right from the start, we had patients advising us.
What we found
We scrutinised findings from 176 trials, which included almost 30,000 patients.
Duloxetine
Our review shows that – despite studies investigating 27 different antidepressants – the only antidepressant we are certain about for the treatmentSomething done with the aim of improving health or relieving suffering. For example, medicines, surgery, psychological and physical therapies, diet and exercise changes. of chronic pain is duloxetine:
- Duloxetine was consistently the highest‐ranked antidepressant, and we are pretty certain this finding can be trusted.
- Standard dose was probably equally effective as high dose for the majority of outcomesOutcomes are measures of health (for example quality of life, pain, blood sugar levels) that can be used to assess the effectiveness and safety of a treatment or other intervention (for example a drug, surgery, or exercise). In research, the outcomes considered most important are ‘primary outcomes’ and those considered less important are ‘secondary outcomes’.. This is important, because we think high doses are more likely to have side effects.
- Duloxetine reduced pain and increased function when used for three common pain conditions: there were a total of 43 duloxetine studies: 11 for fibromyalgia, 18 for neuropathic pain, and 14 for musculoskeletal pain.
- The average length of the trials for all drugs was around 10 weeks, and for duloxetine, was 12.5 weeks, so we still don’t know about any long-term effects.
- We couldn’t find out whether duloxetine (or any other antidepressant) improved mood, because almost all the trials excluded people with low mood and other mental health conditions.
Milnacipran
There is also some promising evidence for milnacipran, but the studies were too few and small for us to be certain about this drug. Milnacipran was often ranked as the next most effective antidepressant after duloxetine, although the certainty of evidenceThe certainty (or quality) of evidence is the extent to which we can be confident that what the research tells us about a particular treatment effect is likely to be accurate. Concerns about factors such as bias can reduce the certainty of the evidence. Evidence may be of high certainty; moderate certainty; low certainty or very-low certainty. Cochrane has adopted the GRADE approach (Grading of Recommendations Assessment, Development and Evaluation) for assessing certainty (or quality) of evidence. Find out more here: https://training.cochrane.org/grade-approach was lower than that of duloxetine.
We have unanswered questions – including a lack of information about long-term effects and side effects
Evidence for all other antidepressants was low or very low certainty. Meaning that there is insufficient evidence to draw robust conclusions about the effectivenessThe ability of an intervention (for example a drug, surgery, or exercise) to produce a desired effect, such as reduce symptoms. and safetyRefers to serious adverse effects, such as those that threaten life, require or prolong hospitalization, result in permanent disability, or cause birth defects. of any other antidepressant for chronic pain.
We also couldn’t assess side effects because these were poorly reported. Our patient advisors told us that they are particularly disappointed about the lack of long-term outcomes with good tracking of side effects because – in their experience – antidepressants are prescribed for longer periods than 10 weeks and are quite hard to get off.
What we have learned: reflections from a clinician
Dr Peter Cole, Consultant in Pain Medicine, Oxford says:
“Of the antidepressant drugs used for nerve pain, fibromyalgia and musculoskeletal pain, we now know that duloxetine has the best chance of helping patients when compared to the other antidepressants.
Duloxetine is also easier to take as there is no need to keep increasing the dose as you often need to with the other drugs. Most people are ok starting on a single dose of 60mg each day, although they may choose to start on a lower dose and increase to 60mg after week or so. There is no need to increase the dose beyond 60mg.
For these reasons of best evidence of benefit and ease of use, duloxetine is the drug that I would recommend starting if patients wanted to trial an antidepressant to see if it helps with their nerve pain, fibromyalgia or musculoskeletal pain. It is really important to keep some sort of diary or record of the benefit and any side effects to determine whether it is worth continuing with the drug. Too many people carry on without reviewing this.
Patients should talk with their own clinician before starting – or changing – the medication they are currently taking for pain. The lack of evidence of benefit from this review for many of the antidepressants for chronic pain does not mean that a particular drug won’t be helpful for an individual patient.
Before starting a new drug, I recommend patients reflect on whether changes to their lifestyle might help when living with persistent pain. This might include increasing their mobility or exercise, their diet or weight loss. Whether their daily routine, hobbies and their sleep could be improved. In addition, there are educational resources and healthcare professionals that can be helpful. I would prefer patients had the opportunity to consider these things before starting a new drug. If they do start a new drug, I’d advise them to review the benefits and side effects and stop taking it if it isn’t helping”.
What we have learned: reflections from a patient
Sarah (not her real name) says:
“I think it’s very difficult for anyone to have an informed decision about which antidepressants they would like to try or try next because there is not enough reliable evidence.
This kind of work, studying the effectiveness of different available antidepressants, should be paramount for informing clinicians – as one in four in the UK populationThe group of people being studied. Populations may be defined by any characteristics e.g. where they live, age group, certain diseases. and a third of the world suffer chronic pain. Not knowing how effective or safe these medications are is a major riskA way of expressing the chance of an event taking place, expressed as the number of events divided by the total number of observations or people. It can be stated as ‘the chance of falling were one in four’ (1/4 = 25%). This measure is good no matter the incidence of events i.e. common or infrequent. to the health of the population. It’s imperative we have further high-quality studies into this, as effectively there are no informed comparisons to help clinicians or patients make decisions.
As a member of the public and a patient who sufferers from chronic pain, I find the dataData is the information collected through research. concerning from an ethical point of view. I believe health care should be as safe as it can be for patients, it should be more strongly based on fact and evidence, with accurate information on what works and what doesn’t – or what is better or worse. Otherwise, I think patients could lack confidence in the health care they receive, and this might also affect their relationship with clinicians. It might also cause people more suffering and for longer.”
What we have learned: reflections from a researcher
Dr Hollie Birkinshaw, senior researcher and lead author of the review, says:
“Considering how common chronic pain is, and the growing criticism of many other drugs (such as opioids, and even paracetamol and ibuprofen), it is not surprising that doctors prescribe antidepressants to reduce pain. The physical systems processing emotions and pain are similar, so theoretically, it makes sense that antidepressants will have an effect.
This review took on a mountain of evidence and wrestled with it to produce trustworthy conclusions. It is disappointing that so much of the evidence is below par.
The good news, that duloxetine appears to reduce pain and increase function in the short term in three major pain groups (fibromyalgia, neuropathic pain, and musculoskeletal pain), is balanced against the gaps in evidence on longer-term use and on harm.”
Reference: Birkinshaw H, Friedrich CM, Cole P, Eccleston C, Serfaty M, Stewart G, White S, Moore RA, Phillippo D, Pincus T. Antidepressants for pain management in adults with chronic pain: a network meta-analysis. Cochrane Database of Systematic ReviewsIn systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. 2023, Issue 5. Art. No.: CD014682. DOI: 10.1002/14651858.CD014682.pub2.
Acknowledgements
This work was funded by the NIHR Health Technology Assessment (HTA) Programme, UK.
Tamar: “With thanks to Cochrane and to the diverse team who worked on this review: a health psychologist, a pain psychologist, a pain physician, an expert in systematic reviews, a clinical pharmacist, a psychiatrist, and an amazing statistician. Gavin Stewart, from Newcastle University led our analysis, using complex methods and wrestling with a mountain of data. Our senior researcher, Hollie Birkinshaw, spent hours making sure that every methodological T was crossed and i was dotted, and writing up a thesis.”



Great article! It’s surprising that there’s still so much we don’t know about using antidepressants for chronic pain management.
Really great to have all three perspectives on this – a really useful read! Thank you!