In this blog, Sarah Rayfield, Speciality Registrar in Public Health, looks at the latest Cochrane evidenceCochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. on vitamin A supplementation for reducing death and disease in children living in low and middle-income countries and asks whether the WHO guidelines need to be updated in the light of it.
Blog updated: 4 April 2022 to reflect an updated version of one of the reviews discussed in the blog ‘Vitamin A supplementation for preventing morbidity and mortality in children from six months to five years of age‘ (published March 2022). No further studies were included in this review and the conclusions remain the same. Further resources have been added to the blog. Page last checked 14 March 2023
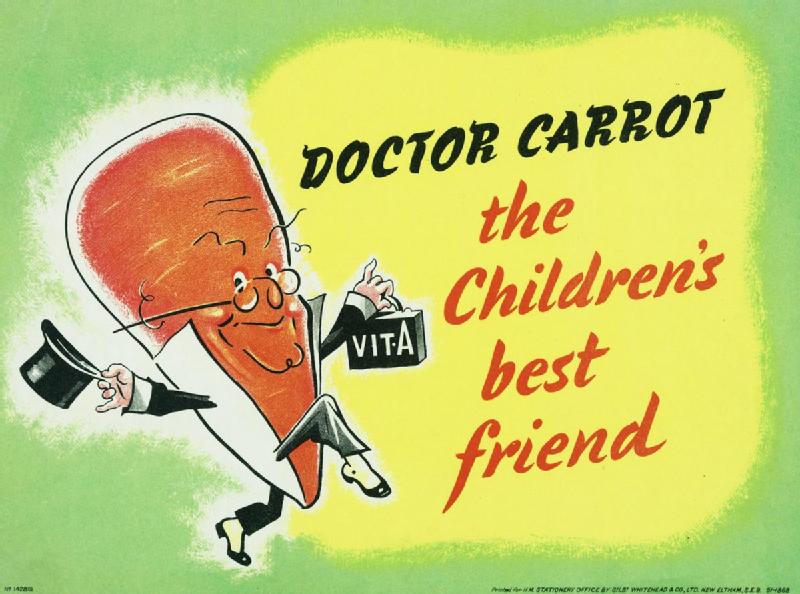
“Carrots help you see in the dark!” was a popular saying in England during the Second World War. Doctor Carrot depicted with his bag of vitamin A was proclaimed as the “children’s best friend”. We now know that although vitamin A may not actually help you see better in the dark, it is indeed highly necessary for eye health with vitamin A deficiency being a leading cause of preventable blindness in children worldwide. In fact, Vitamin A is an essential nutrient needed for growth and maintenance of all the normal functions of the human body and children who do not have enough of it are at a much greater riskA way of expressing the chance of an event taking place, expressed as the number of events divided by the total number of observations or people. It can be stated as ‘the chance of falling were one in four’ (1/4 = 25%). This measure is good no matter the incidence of events i.e. common or infrequent. of dying from serious infections.
Since 2011, the World Health Organization (WHO) has recommended universal vitamin A supplementation for children aged between 6 months and 5 years who live in areas where vitamin A deficiency is present (WHO, 2011). These recommendations were based on two previous Cochrane ReviewsCochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research., both of which assessed the evidence for vitamin A supplementation in reducing death and disease but one looked at children in general, with the other review looking at adults and children with human immunodeficiency virus (HIV).
The first of these two reviews Vitamin A supplementation for preventing morbidity and mortality in children from six months to five years of age was updated in 2022 and a further two Cochrane Reviews published which ask the same question but for different ages – newborn babies born at term (Neonatal vitamin A supplementation for the prevention of mortality and morbidity in term neonates in low and middle income countries; published February 2017) and for infants aged 1 to 6 months of age (Vitamin A supplementation for the prevention of morbidity and mortality in infants one to six months of age; published September 2016). This blog considers the evidence assessed by all three of these reviews and asks – does the WHO guidelines need to be updated in light of this evidence?
Vitamin A supplementation: new evidence
The updated review Vitamin A supplementation for preventing morbidity and mortality in children from six months to five years of age (updated April 2022) looking at children aged 6 months to 5 years, continued to find that vitamin A supplementation reduced the risk of death from all causes by 12%. This was mostly due to the reduction in incidenceThe number of new occurrences of something in a population over a particular period of time, e.g. the number of cases of a disease in a country over one year. and death from diarrhoea. Vitamin A supplementation may not reduce the risk of death from measles, respiratory disease or meningitis. There was also evidence that supplementation probably reduces the number of children with Bitot’s spots (a sign of vitamin A deficiency) and the number of children who develop night blindness.
Conversely, for newborn infants and infants aged between 1–6 months of age, neither Cochrane Review found reliable evidence that vitamin A supplementation at these ages reduced the risk of death or illness from any cause by either 6 months or 1 year.
For newborn infants, there was also no evidence that vitamin A supplementation from birth reduced the likelihood of vitamin A deficiency at either 6 weeks or 4 months of age. Although there was probably no evidence of increased side effects such as vomiting or diarrhoea, babies who had vitamin A supplementation were more likely to have a bulging soft spot on their heads (fontanelle) in the first 2-3 days after starting supplements. In fact, infants aged 1-6 months who were given vitamin A, were found to have three times the risk of a bulging fontanelle when compared to those who did not receive vitamin A. Although this did not increase the risk of death or seizures, it is unlikely to be an acceptable side effectAny unintended effect (e.g. dizziness or a headache) of an intervention such as a drug, surgery or exercise. in the light of no evidence of clinical benefit.
The Cochrane Review looking at newborn infants did suggest that while the combined result showed no evidence of effectivenessThe ability of an intervention (for example a drug, surgery, or exercise) to produce a desired effect, such as reduce symptoms., there was an indication that individual studies showed vitamin A supplementation to be more effective when given to children in countries with higher levels of vitamin A deficiency (such as in Asia). However, giving vitamin A to infants in areas with less deficiency (such as in Africa) did not reduce the risk of death and, in fact, appeared to have caused harm through side effects. However, the authors caution the need for further evidence before policy changes are made on the basis of these particular results.
How reliable is the evidence?
Each of the three reviews included studies of children living in low and middle-income countries, which is appropriate given the global distribution of vitamin A deficiency. The newborn review contained 12 studies and over 168,000 infants. In general, the quality of evidence was high except for outcomesOutcomes are measures of health (for example quality of life, pain, blood sugar levels) that can be used to assess the effectiveness and safety of a treatment or other intervention (for example a drug, surgery, or exercise). In research, the outcomes considered most important are ‘primary outcomes’ and those considered less important are ‘secondary outcomes’. of diarrhoea immediately following starting supplements and when the authors looked at risk of death at 6 months in term infants only. The review looking at infants aged 1-6 months also included 12 studies with just under 25,000 infants. The quality of the evidenceThe certainty (or quality) of evidence is the extent to which we can be confident that what the research tells us about a particular treatment effect is likely to be accurate. Concerns about factors such as bias can reduce the certainty of the evidence. Evidence may be of high certainty; moderate certainty; low certainty or very-low certainty. Cochrane has adopted the GRADE approach (Grading of Recommendations Assessment, Development and Evaluation) for assessing certainty (or quality) of evidence. Find out more here: https://training.cochrane.org/grade-approach in this review was more mixed with most studies considered to be of low or moderate quality, usually due to the risk of biasAny factor, recognised or not, that distorts the findings of a study. For example, reporting bias is a type of bias that occurs when researchers, or others (e.g. drug companies) choose not report or publish the results of a study, or do not provide full information about a study..
The review on children aged 6 months to 5 years was the largest and included 47 studies with over 1.2 million children. Again the quality of the evidence was mixed with the authors assessing most studies to be of low or moderate quality. Although bias was felt to be an issue in some studies, it was judged that the main outcome of the impact of vitamin A on reducing death was at low risk of bias.
What does this change about what we know?
In essence, these recent Cochrane Reviews show that the current WHO policy is in line with current evidence. There was no evidence of clinical benefit when giving vitamin A to newborn infants, or those up to 6 months of age. In fact, supplementation at these early ages only appeared to increase the risk of side effects. There is currently only evidence for benefit of vitamin A supplementation in those aged 6 months to 5 years and it is indeed an important benefit – reducing the risk of death, particularly from diarrhoeal illness. According to the WHO, diarrhoeal disease is the second leading cause of death in children worldwide under the age of 5 years and it is also a leading cause of malnutrition in this age group (World Health Organisation, 2017). Vitamin A supplementation, therefore, has an important role to play in reducing this burden of disease.
Given that we know vitamin A supplementation to be effective in those aged 6 months – 5 years, considerations should turn to ensuring the universal supplementation programme is delivered in the most practical and cost-effective way to all children living in areas of vitamin A deficiency.
As vitamin A is a fat-soluble vitamin it can be stored in the liver which means it is only needed every 6 months to avoid deficiency. Currently, many countries have developed strategies to integrate vitamin A supplements into routine health services, or distributing alongside national immunisation programmes (Unicef, 2007). However, in order to be truly effective, there needs to be wide-ranging interventions to improve child health which include the promotion of vitamin A-rich diets, food fortification and ensuring breastfeeding, alongside universal vitamin A supplementation.
Further information
- Cochrane Clinical Answer: What are the effects of vitamin A supplementation on mortality and morbidity among neonates in developing countries?
- Cochrane Clinical Answer: In infants up to six months of age, how does vitamin A supplementation affect morbidity and mortality?
- UNICEF. UNICEF Data: monitoring the situation of children and women – Vitamin A deficiency
- BMJ Global Health: Refocusing vitamin A supplementation programmes to reach the most vulnerable.
Sarah Rayfield has nothing to disclose.


